CareCentric: Shared Care Record Solution
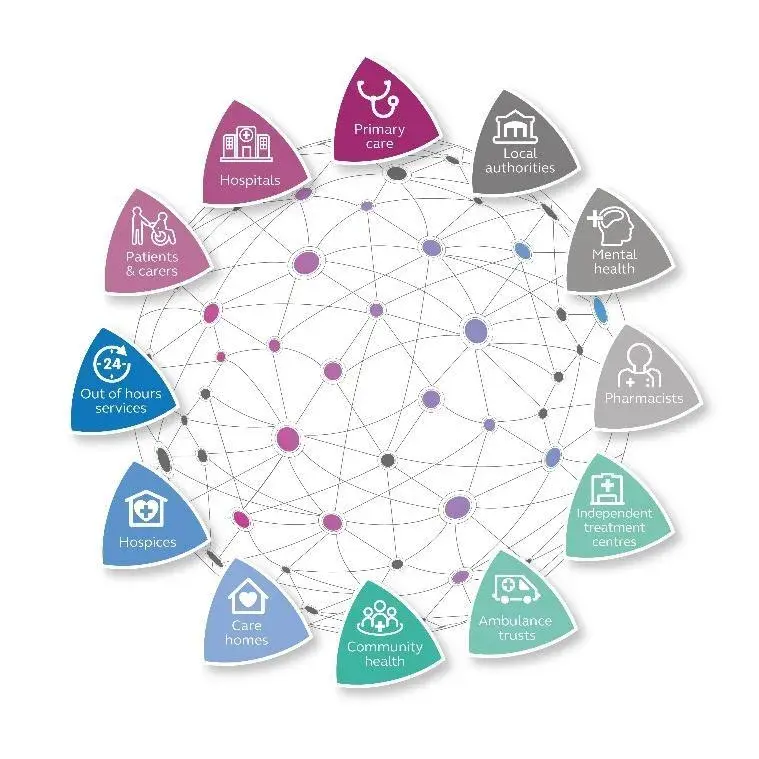
Our CareCentric record-sharing solution is designed to improve and deliver joined-up health and social care services for Integrated Care Systems (ICS) in the UK.
Trusted by hospitals, councils and other organisations within Integrated Care Systems (ICS), CareCentric has been developed by industry experts to help tackle health inequalities, reduce hospital admissions, improve patient engagement, join up health and social care, prevent major health issues, and solve the waiting list problem.
As the leading provider of shared care records in the UK, Graphnet Health work with commissioners across the country to provide over 20 million individuals with better, faster and more joined up care.
What is a Shared Care Record?
CareCentric is a cloud-based platform that combines health and social care data from multiple disciplines to create a single, secure Shared Care Record.
Shared Care Records allow data to be drawn from and shared between a variety of sources, including:
- Acute Hospitals: patient demographics, referrals, attendance (inpatient/outpatient, A&E), waiting list, medications, alerts, allergies, pathology results and radiology reports
- GP Practices: patient demographics, diagnoses, treatments, medications, allergies, results, disease register, co-morbidities and family history
- Community and Mental Health: patient demographics, care plans, problems, interventions, medical and social alerts, medications, referrals and clinical summaries
- Social Care: care teams, keyworkers, contacts and other involvements, assessments, needs and care provision details
Relevant information can then be accessed and updated in real time by authorised people involved with the patient’s care. This improves digital communication and collaboration, allowing clinicians to deliver more efficient patient-centred care planning.
CareCentric Features
- Cloud-based platform. CareCentric is cloud-hosted to ensure scalability, resilience, and security. Data is processed in the Microsoft Azure cloud platform, on UK-based servers.
- Interoperable. The platform connects with all major health and social care IT systems in the UK, with API portals available for third-party applications.
- Single Sign-On. SSO gives authorised users direct access to patient records within their existing IT system, reducing admin time and improving efficiency.
- Mobile. The platform is available on smartphones and tablets as well as desktop PCs, allowing care professionals to access and capture patient data wherever they need to.
- Comprehensive digital care record. Our fully integrated records collate and display data from diverse care sectors within the community, including hospitals, GPs, community care and social care.
- Integrated care plan. CareCentric supports coordinated workflow management across multi-disciplinary teams, providing true patient-centred care planning.
How does it work?
CareCentric can operate at any of the four Shared Care Record levels – from an integrated record viewer to a complete cross-organisational care planning solution.
- Level 1: Sharing information
Our fully integrated digital care record combines data from multiple types of organisation and across care settings within a designated community.
- Level 2: Care planning support
At level 2, CareCentric also supports the collection and update of community-wide assessment, event-driven alerting, task management, referral, secure instant messaging, workflow and care planning applications.
Patient registers can be created using risk stratification or manual assignment. Care plans can be tailored to suit a wide range of requirements, including condition management (for example: COVID-19, frailty, heart failure) and end of life preferences.
- Level 3: Patient access and engagement
At this level, patients also have access to their own shared care record: myCareCentric Personal Health Record. This means they can update their own personal information and contact details, self-monitor using wearables and telehealth devices, and interact directly with clinicians in real-time to improve the management of their condition.
- Level 4: Population health management
At the top level, CareCentric can also be connected to our Population Health Management software to provide data-rich analytics and wider population health intelligence.
The platform allows for the analysis of aggregated patient data gathered from across a care community, using risk stratification and other tools. This can be provided in an anonymised, pseudonymised or plain form, depending on data-sharing agreements.
Case Studies
Read about our development work on the Greater Manchester Care Record (GMCR) – a CareCentric digital shared record that combines patient data for 2.8 million citizens and is being used by health and social care professionals across the region’s 10 localities.
"CareCentric is well-liked and used by clinical staff in our Trust and across the Dorset community.”
Tracie Tiller, applications programme manager, Bournemouth & Poole Informatics Service