Population Health is a vital tool for targeted direct care
14 July 2023
By David Grigsby, Graphnet Health
Everyone knows that the funding increases that the NHS needs and wants will not be forthcoming, and - if it wants to maintain and improve service - it must transform. Integrated Care Boards (ICBs) are increasingly recognising the power of data to transform the way that care is delivered. By harnessing the potential of data analytics and population health management, the NHS can maximise resources and achieve better outcomes for patients. In this article, we explore the importance of using data to identify cohorts of people that will benefit from proactive, focused, early intervention; and how this can achieve better outcomes and save money.
How population health management and data is helping tackle elective recovery.
The 2023/24 NHS priorities and operational planning guidance listed elective care as a core recovery and productivity planning objective. The benefits of using data to support that requirement are obvious when you look at organisations like Buckinghamshire Healthcare NHS Trust, which has collaborated with Graphnet to create a digital solution to support the transformation of their peri-operative pathway - seen as being a key factor in increasing productivity in the elective pathway. It is believed to be the first example in the UK using digital integration to combine surgical waiting lists with primary care records. By integrating the shared care record with Patient Treatment Lists (PTLs) they are able to identify low and high-risk surgical patients, with the dashboard performing automatic clinical stratification of those patients.
This has already proven to have significant time and resource savings. For example, by taking into account the wider morbidity profile of patients, available through primary care data, the identification of high-risk patients is easier and more efficient. Surfacing these insights through a dashboard has enabled essential prehabilitation pathway transformation without significant additional expenditure.
Patients can quickly be identified and sent a variety of communications specific to their chronic health condition with related information and clinical advice. The aim is to optimise patients for surgery and reduce the likelihood of cancellations. Candidate lists for cancellations with a curated patient profile available to review have also meant that the time spent trying to fill cancelled slots has decreased as patients can be targeted more easily. The analysis supports the triage of patients to the most appropriate pre-op assessment, again helping to support the unblocking of bottle necks in the perioperative pathway.
Validation opportunities are also highlighted with the ability to identify those patients who are deceased or have moved addresses.
Transforming care in primary and secondary care through remote digital management and proactive disease cohort identification.
Last winter saw further pressure on emergency and urgent care services in acute hospitals. The priorities and operational planning guidance called out the need to decrease occupancy by increasing patient flow and enabling medically fit for discharge patients to be discharged faster. One key method to support this aim has been through the use of remote monitoring (virtual wards) and increasing capacity within community hospitals.
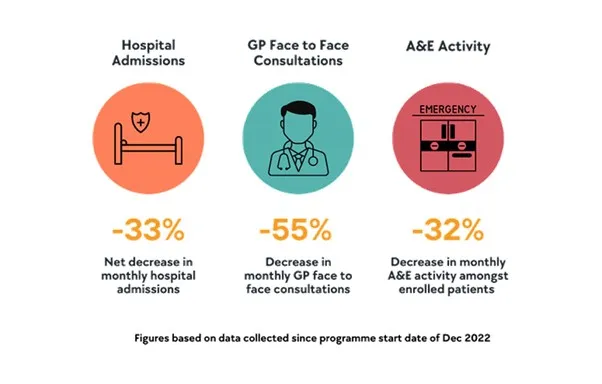
The Frimley Integrated Care System Connected Care programme uses Graphnet’s population health management platform to create analytics that segment and stratify their population, allowing them to identify their most complex and frail patients using both primary and secondary care data. Suitable impactable cohorts are identified through clever cohorting analytics and referred to Docobo for proactive remote monitoring and virtual ward services. Since the programme started in December 2022, there have been some outstanding results:
Working towards equity and optimising the care of vulnerable patients.
The NHS Core20PLUS5 approach identifies key target areas where equity in health and care needs to be accelerated.
The Graphnet population health management tools are supporting ICSs across the country with delivery of equity through analytical insight. These include a focus on improving the life expectancy of patients with a serious mental illness through caseload lists that identify candidates for health checks; quantifying the demographic influencers that affect vaccination rates in pregnant women; and innovative projects that have been developed to help tackle fuel poverty by medically optimising patients and prescribing heat.
Cheshire and Merseyside ICB created a fuel poverty dashboard in their Graphnet hosted population analytics platform, CIPHA, analysing GP data, deprivation, Johns Hopkins risk of admission prediction scores and fuel poverty data profiles to identify patients with chronic respiratory disease and asthma who may deteriorate due to the effects of fuel poverty. In St Helens, the COPD team are using the fuel poverty analytics to offer high-risk patients face-to-face reviews. It is still early days but, as of May 2023, there have been 49 referrals to the Wellbeing Team and 49 referrals to the Affordable Warmth Team (AWT). Out of the AWT referrals, 69% have received payments from household support funds, to help them keep their homes warm and healthy. The aim of this pilot programme is to blueprint it and use it as a model of good practice to support people at risk over winter.
Conclusion
The NHS faces numerous challenges in delivering high-quality care while managing limited resources. Embracing the power of data and advanced analytics is key to overcoming these challenges. By identifying cohorts of people in need of early and focused interventions, the NHS can maximise its resources, improve patient outcomes, and reduce healthcare costs. Graphnet Health's population health and shared care IT systems play a crucial role in enabling this data-driven approach, providing healthcare professionals with the tools necessary to deliver efficient, patient-centric care. Through strategic collaboration between healthcare providers and technology experts like Graphnet Health, the vision of a data-powered NHS that achieves better outcomes for all can become a reality.
For more information about Graphnet’s population health management tools, visit this page.










